What causes IBD?
 While the exact cause of IBD is not known, it is believed to be brought on by an interaction between your genes, gut bacteria (microbiome), the environment and your immune system. Scientists have identified >160 points in human DNA that can have genes which increase your likelihood of getting IBD. Some of these are associated with Crohn’s disease, others are linked to UC, but the majority of them are linked to both diseases. However, having a genetic predisposition is not enough. The environment also plays an important role in IBD. If a person who is genetically predisposed is exposed to these environmental factors, these genes can be triggered and the immune system can start attacking its own GI tract. Environmental factors that have been proposed are smoking, diet, sanitation, the use of antibiotics, and even an infectious gastroenteritis. There is ongoing research to figure out exactly how this happens. IBD is not contagious, however due to your shared environment and genetics with your family, your parents, siblings and children have an increased risk of also having IBD.
While the exact cause of IBD is not known, it is believed to be brought on by an interaction between your genes, gut bacteria (microbiome), the environment and your immune system. Scientists have identified >160 points in human DNA that can have genes which increase your likelihood of getting IBD. Some of these are associated with Crohn’s disease, others are linked to UC, but the majority of them are linked to both diseases. However, having a genetic predisposition is not enough. The environment also plays an important role in IBD. If a person who is genetically predisposed is exposed to these environmental factors, these genes can be triggered and the immune system can start attacking its own GI tract. Environmental factors that have been proposed are smoking, diet, sanitation, the use of antibiotics, and even an infectious gastroenteritis. There is ongoing research to figure out exactly how this happens. IBD is not contagious, however due to your shared environment and genetics with your family, your parents, siblings and children have an increased risk of also having IBD.
What is going on in my body?
The inflammation in IBD is signaled to occur via an imbalance or trigger in your immune system that causes immune cells (white blood cells) to attack your GI tract lining – this is why it is considered an autoimmune disease (your body is recognizing your intestine as foreign and reacting to it). The immune cells also release pro-inflammatory cytokines (eg. TNF-alpha). Cytokines are little proteins that tell other cells what to do – and, in this case, it tells them to be inflamed, which causes damage and prevents healing. This is why many IBD medications target the cytokines, or the receptors on other cells that allow white blood cells to invade the tissue. Because both of these diseases involve an increased inflammatory response in your body, the inflammation can travel to other organs or systems.
Symptoms of diarrhea and pain are common in IBD because the wall of the intestine is being damaged and this disrupts your digestion and can cause swelling and irritation. People may start to lose weight if they cannot eat normally and are having many bowel movements per day. Fatigue is also common, because not only is it tiring to be in pain and have to go to the washroom frequently, but the ongoing inflammation is physically demanding on your body.
Specific information about Crohn’s disease and ulcerative colitis is described below.
To TopCrohn's Disease
In Crohn’s Disease, your immune system is upregulated and can cause inflammation to occur anywhere along your GI tract, from your gums to your bum. Crohn’s disease tends to have “skip lesions” – where several parts of your intestine may be affected but the intestine in between is normal. If you do not know which part of your intestine is affected, ask your gastroenterologist. The inflammation in Crohn’s disease can affect all of the layers of the GI tract wall (we call this transmural disease), which is why you may develop stricturing or penetrating (abscess or fistula) disease. It is currently estimated that approximately half of patients with Crohn’s disease will develop a complication, like a fistula or stricture, within 20 years of their diagnosis.

What is stricturing disease?
A stricture is a narrowing of the intestine, which can lead to a blockage of the intestine, where the intestinal contents (or partially digested food) is not able to pass through. Strictures are more common in the small intestine, but can also affect the large intestine. A stricture can be inflammatory or “fibrostenotic” or a combination. An inflammatory stricture may respond to medications that are used to treat Crohn’s disease, however fibrostenotic strictures are due to scar tissue and generally respond poorly to medications. Strictures in Crohn’s disease usually show thickening of all layers of the intestine. Strictures can also occur at a site of a previous surgery on your intestine (called an anastomosis). See IBD Procedures, Imaging & Surgeries for more information.
Strictures of the intestine can cause symptoms of intermittent abdominal pain, bloating, or even bowel obstruction – this can lead to nausea and vomiting. If you have symptoms that suggest you have a stricture and are unable to keep food down, you should seek medical attention right away.

What is penetrating disease?
Penetrating disease is when the disease penetrates through the layers of the intestine to create either a fistula (passage between the lumen of the bowel and another surface), or an abscess (collection of pus) or a phlegmon (an inflammatory mass, that may or may not have an abscess with it). A large abscess requires drainage along with treatment with antibiotics. If the abscess is small, we treat it with antibiotics (plus, other treatments for your Crohn’s disease).
Fistulas (or passage ways) are tracts between the intestine and another surface and they are named by the two surfaces they connect. For example, fistulas that extend from the small bowel, start with the prefix “entero-” and fistulas from the large intestine start with the prefix “colo-”. The common types that are seen in Crohn’s disease are: between the intestine (e.g. entero-enteral, enterocolonic), to the skin (-cutaneous), bladder (-vesicular), and vagina (enterovaginal). Perianal fistulas are a special type of fistula to the skin around your anus. See IBD Procedures, Imaging & Surgeries for information on how this is treated.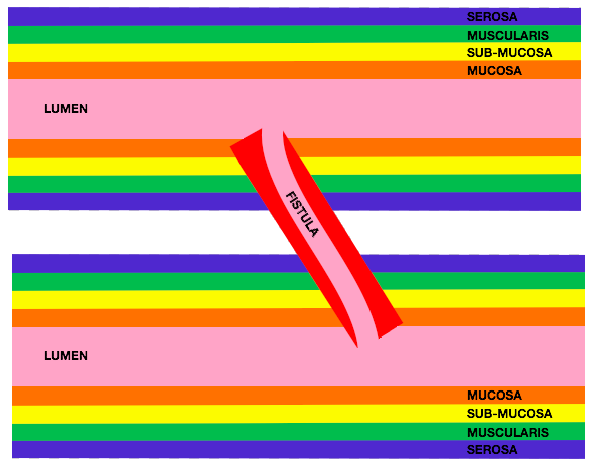
To Top
Ulcerative Colitis
In ulcerative colitis (UC), your immune system is upregulated and can cause inflammation to occur in your large intestine, also called your colon. The type of inflammation in this disease only affects the inner layer inside of the large intestine, called the mucosa. UC always starts in your rectum and extends up into your large intestine from there. This means that, unlike Crohn’s disease where there are “skip lesions,” the diseased sections of the large intestine are in contact with areas of diseased bowel further down the tract. Part of the assessment of UC is to determine the disease extent, or how much of the large intestine is diseased (see diagram).

Flares
If you develop symptoms of active IBD, like abdominal pain, diarrhea, rectal bleeding, you may be experiencing a flare. You should seek medical attention – call your family doctor’s office and make an urgent appointment or call your gastroenterologist’s office and talk to the IBD nurse or make an urgent appointment. It is important to determine if your symptoms are related to a flare of your IBD or are due to other factors – e.g. antibiotics, irritable bowel syndrome, etc.
Flares can happen for a variety of reasons, and can differ from person to person. Common causes of flares are:
- Infection (this could be a bacterial infection (food poisoning), a flu, or an infection called difficile)
- Not taking your medication(s) properly or running out of them
- Certain medications, like NSAIDs (non-steroidal anti-inflammatory drugs) may cause some patients with IBD to flare
- Stress – it is important to stay aware of your mental well-being and to try to maintain balance because stress or anxiety can negatively impact your ability to stay healthy. For more information on this, see Living with IBD.
- Loss of response to medications – sometimes your disease will stop responding to the medications you are taking; we call this “loss of response”
- Disease progression – sometimes your IBD may progress in severity and you may require stronger medications (for example, this may happen if you are on a steroid taper and as you decrease your dose, it may no longer be enough to keep you well)
It would be helpful for you to take note of events (changes in medications, contact with another person that is sick, etc) that preceded a flare so you can figure out over time what the triggers might be for you.
To TopPrognosis and Potential Complications
Prognosis: Life expectancy for people with IBD is similar to that of people who do not have IBD; however, IBD is associated with some complications that may increase risk of death. Other complications of IBD may affect your quality of life (also called morbidity). In addition, medications for IBD may lead to complications.
Complications associated with increased mortality:
- Malignancy/cancer: Colorectal cancer risk increases with increased disease duration, severity of inflammation and family history of colorectal cancer.
- Toxic megacolon: A severe case of colitis can lead to further inflammation of the large intestine which could cause toxic megacolon (where your colon is very inflammed, becomes enlarged and could rupture), which can lead to sepsis (blood poisoning with harmful bacteria).
- Thrombosis: Blood clots can occur inside the body and are named differently depending on where they happen (e.g. in the lung it would be a pulmonary embolism, in the brain it would be a stroke, in your leg it is a deep vein thrombosis [DVT]). People with active IBD are at increased risk for thrombosis. If you are admitted to hospital with a flare of your IBD, a type of medication called heparin or low-molecular weight heparin (LMWH) will be prescribed to reduce your risk of clots.

- Infection: Patients with IBD have an increased risk of infection and this can sometimes lead to mortality. Some of the medications used to treat IBD suppress your immune system leading to this increased risk. IBD patients are vulnerable for an infection of the bowel, called Clostridium difficile or “C. diff.”
Other Complications:
- Nutrient deficiencies: Most commonly in iron, vitamin D, vitamin B12 and calcium. People with IBD may have lower levels of nutrients if they have areas of the intestine that are not able to absorb nutrients well, are missing segments of their GI tract due to resections or colectomy, are unable to consume enough nutritious food or are experiencing chronic diarrhea or bleeding.
- Growth failure: If a child is experiencing chronic active disease, they may be lacking some of the aforementioned nutrients and their bodies may not be able to keep up with the metabolic demand required by their disease and growing at the same time. Consequently, young adults who have had frequently active disease may have had a delay in growth or may not have had long enough stretches of remission to reach their optimal growth rate.
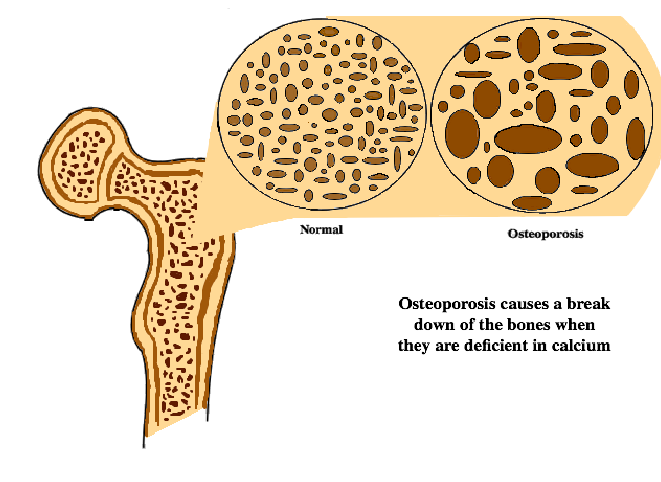
- Osteoporosis: This is a weakening of the bones, which can be brought on by long-term use of corticosteroids or deficiencies in calcium and vitamin D – in these circumstances your system starts to break down your bones instead of building them up.
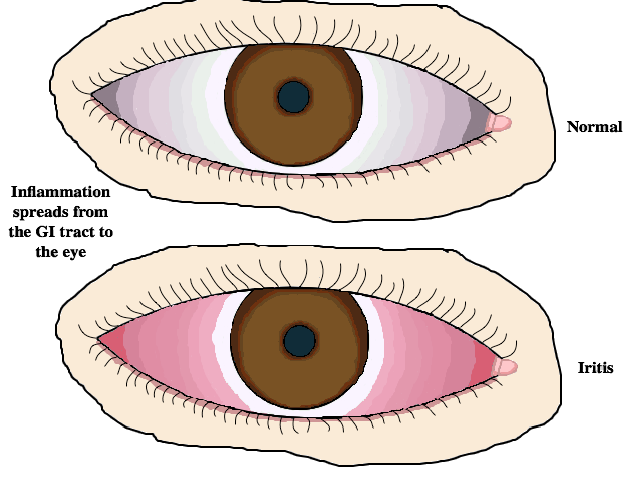
- Extraintestinal manifestations: The inflammation that occurs in your GI tract can spread to other areas of the body outside of the intestine (extraintestinal). This can lead to problems with joints such as inflammation or arthritis, eye inflammation, skin rashes, or diseases with other organs such as your liver, pancreas or kidneys.
- Iritis: This is a common eye complication for patients who suffer from IBD. The inflammation spreads from the GI tract and affects the iris of the eye. There are usually slight pains associated with iritis, as well as redness and possibly even blurry vision.
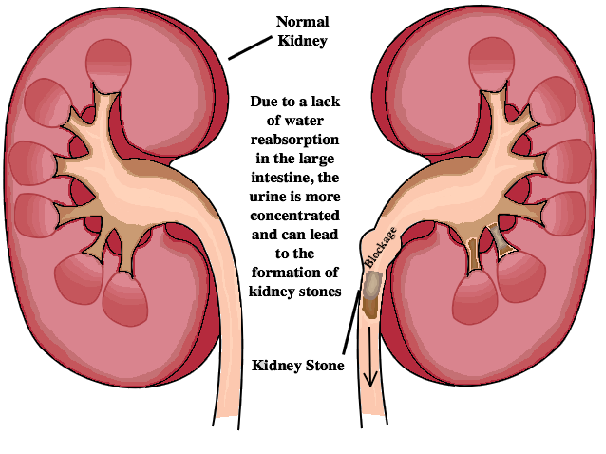
- Kidney Stones: After several small resections of the bowel, it becomes more likely for a patient with IBD to form kidney stones. The lack of water reabsorption causes the urine in the kidneys to be more concentrated creating a higher chance for kidney stone formation. Symptoms may include pain, vomiting, and blood while urinating.
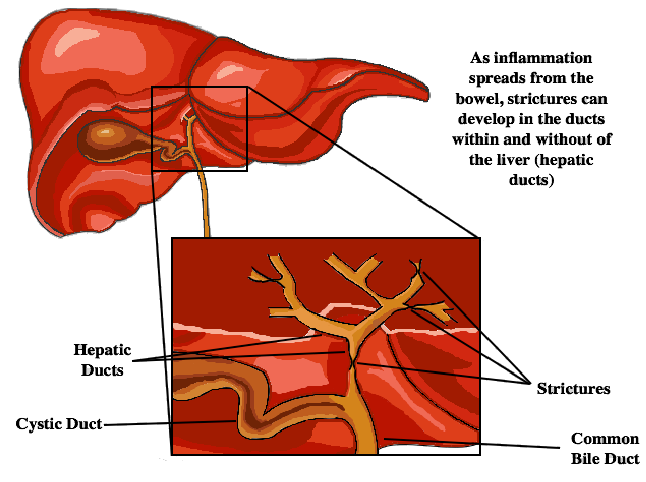
- Primary Sclerosing Cholangitis: If inflammation spreads to the gallbladder, the ducts connecting the liver to the gallbladder and the gallbladder to the small intestine can be blocked. The ducts can develop strictures that prevent bile from getting to the gallbladder and the small intestine. In more severe cases, this can lead to cirrhosis and liver failure.
Anatomy of the GI tract

The gastrointestinal (GI) tract is made up of (in order):
- mouth/oral cavity (including your tongue, as well as hard and soft palate/gums) which starts the breakdown of food by chewing, salivary enzymes and the creation of a food bolus which you swallow.
- esophagus which uses peristalsis to allow you to swallow the food bolus or any liquid.
- stomach, which is where a lot of the mechanical, mashing and mixing digestion of food happens, as well as the breakdown of proteins and other nutrients by the stomach acid.
- small intestine (this is divided into 3 parts: duodenum, jejunum and ileum) is the longest part of the GI tract where many nutrients are absorbed from the digested material (chyme) that enters. It is here that bile enters your digestive system through the bile duct from the gallbladder (where it is stored) to help with the digestion of fats and vitamins.
- colon/large intestine (this is divided into 5 parts: ascending, transverse, descending, sigmoid, and rectum) is where much of the water is absorbed from the chyme to create a formed stool by the end of the bowel. The very beginning of the colon is called the cecum and the end is the sigmoid region.

- rectum ends in a ring of muscle which lets you know/gives you the urge that it is time to pass stool.
- anus is the final opening through which your stool passes to be expelled outside of your body.
There are several solid organs that are part of the GI tract:
- liver filters blood coming from the digestive tract to remove any toxins. The liver creates bile and stores many nutrients that have been digested.
- gallbladder stores the bile created by the liver until it is needed.
- pancreas produces digestive enzymes. It also secretes insulin to help the body absorb sugar after eating.
To Top
Procedures, Imaging & Surgery
Endoscopy Procedures
Endoscopy is performed to diagnose and monitor disease – a camera on the end of a flexible tube is extended into your body through an orifice (entrance to the body). Endo means inside, which makes sense because the purpose is to see the inside of you. The main types of endoscopy used in gastroenterology are described below. Depending on your disease type/location, you may have had one or all of these types.

Preparation: You will be given instructions on how to prepare for the procedure – read them carefully. Preparation for a colonoscopy includes 3 parts:
- Drinking only clear fluid for the day prior to the procedure – you must not eat solid food when you are preparing. You should also avoid seeds, corn, peas, tomatoes, and grapes for 3 days prior.
- You will be asked to take a “bowel preparation” where you must drink a powerful laxative starting the day before to empty your bowels so that the gastroenterologist can see the walls of the intestine clearly. It is important not to schedule anything once you start the preparation, so that you can be home and near a toilet.
- Fasting – you need to be fasting for at least 2-4 hours prior to your appointment.
Procedure: When you arrive at the hospital or endoscopy centre, you will be asked to change into a gown and an IV will be started. You are usually sedated for these procedures, with medications called “conscious sedation”. The common medications used for this type of sedation include: midazolam, fentanyl, and propofol. The purpose of the sedation is to keep you comfortable during the procedure and allow you to recover quickly after the procedure. During the scope, they may take samples of your tissue so the gastroenterologist can send it to be analyzed – these are usually very small pieces.
Post-procedure: You need to be accompanied home from the procedure, if you have been sedated. You are not allowed to drive or operate heavy machinery until the next day. Some people might experience excess gas after the procedure – walking often helps you to pass this.
- Colonoscopy: The endoscope is inserted through the anus/rectum and advanced through the large bowel/colon, usually all the way into the last part of the small intestine (ileum) which attaches to the colon at the cecum.
- Sigmoidoscopy: The endoscope is inserted through the anus/rectum and advanced only into the lower part of the colon – the sigmoid region. The prep for this procedure may not be as extensive as for the colonoscopy.
- Gastroscopy: The endoscope is inserted through the mouth and advanced all the way through your esophagus, stomach and into the first part of the small bowel (duodenum). The prep for this procedure is only fasting.
- Small bowel (Balloon-Assisted Enteroscopy): This is a newer procedure and is not done as frequently unless there is suspicion that you have disease in the small bowel. It is difficult to maneuver into this area of the GI tract, so a scope with 1 or 2 balloons attached to the end is used to traverse through the tract.
- Capsule Endoscopy: This is a procedure, where you swallow a pill-shaped capsule with a camera in it, which sends pictures to a recording device that you wear on your body during the test. It is used to visualize the small bowel and takes many pictures as it travels through you. This is used to look for ulcers and inflammation in your small intestine.
Imaging (Radiology Tests)
Various types of medical imaging might be necessary during your lifetime. These pictures are necessary to assess disease extent/severity or the location of a stricture. Most often, you will either be requested to go for a CT Enterography or an MR Enterography. An enterography is a scan that is designed to look at the intestine – you will be asked to drink a solution right before the test to distend the lumen and you will receive contrast through an IV. An enterography can be done with either an MRI scanner or a CT scanner.
- CT stands for computed tomography. A CT scan uses X-ray beams and causes radiation exposure. A CT scanner captures the images faster and so can lead to better resolution of the intestine.

- MRI stands for magnetic resonance imaging. It does not use X-ray beams and therefore does not lead to radiation exposure. An MRI scanner is slower and therefore the pictures of tissues that move (like the intestine) may be harder to see.
- Ultrasound (with or without contrast) can also be used to detect disease activity. Ultrasound uses sound waves to create the image, so there is no radiation exposure.
Surgeries
Surgery is sometimes used in the treatment of IBD. It is often reserved for occasions when other medical therapies have failed, but it really depends on your specific circumstance and personal preferences.
The types of surgeries in ulcerative colitis include:
- Colectomy: This surgery is done to remove the entire large bowel/colon, mostly in ulcerative colitis patients with chronic active disease. If the rectum is also removed, this is called a proctocolectomy. People who have their colon removed will either have a permanent ileostomy or ileo-anal pouch.
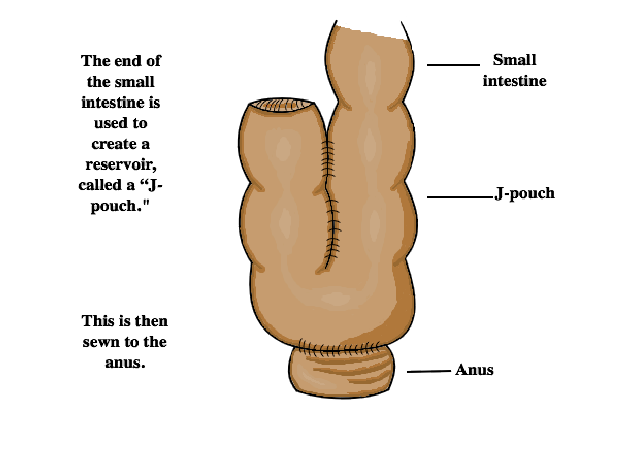
- Ileo-anal pouch/J-pouch: This is done after a colectomy, usually in individuals with ulcerative colitis, to form a place for stool to collect and so the person can control when it is excreted (instead of having an ileostomy).
The types of surgeries in Crohn’s disease include:
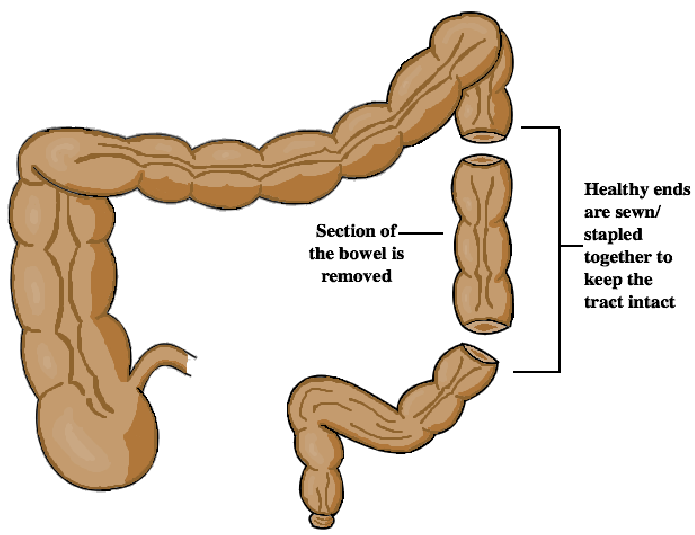
- Resection: This can be done when part of the bowel is so badly affected by disease, (for example, in the case of a fibrostenotic stricture) that it must be removed and the healthy ends will be sewn/stapled together (anastomosis) to keep the tract intact. The name of the resection will depend on what part of the bowel it removes.
- Stricturoplasty: For a shorter fibrostenotic stricture, the stricture can be cut open and sewn back width-wise to create more space for things to pass through without removing any of the intestine.
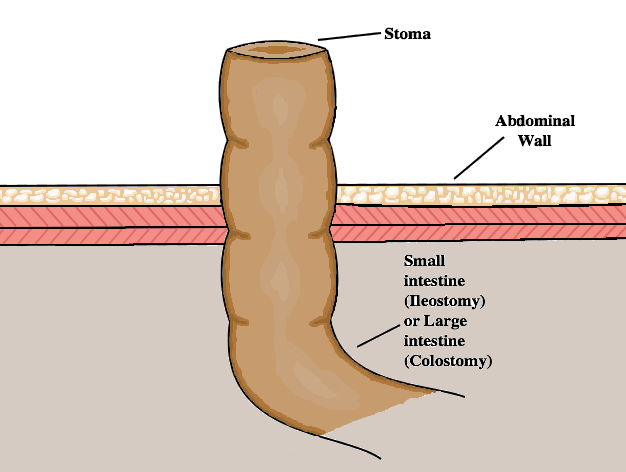
- Ileostomy: After a colectomy, the end of the small intestine can be brought to the surface of the abdomen and sewn there. A bag will be attached to capture the gas or excretions of the small bowel. The opening on the surface of the abdomen is called a stoma. People who undergo this procedure will receive training and usually have access to a stoma nurse to help support them in this transition.

- Colostomy: If, after a partial colectomy, some of the large bowel/colon is still intact, it will be drawn toward the surface of the abdomen and stitched there. A bag will be attached to capture the gas or excretions of the bowel. The opening on the surface of the abdomen is called a stoma. People who undergo this procedure will receive training and usually have access to a stoma nurse to help support them in this transition.
The treatment of perianal fistulas usually involves an operation called: Examination under anaesthesia (EUA). At an EUA, the colorectal surgeon may do one of the following procedures to treat your fistula.
- Fistulotomy: The surgeon will cut along the fistula pathway so that it heals in on itself. This is only for very simple, or low-lying fistulas – it is important that the sphincters or muscles that contract to keep you in control of your bowels are not damaged.
- Setons: If a fistula passes through the anal sphincter muscles, the surgeon may not want to risk damaging the muscle and will instead pass a seton (plastic thread) through the tract and tie it in a loop on the outside so that the fistula can remain open to drain. This will help prevent abscesses, which can form when the end of a fistula closes and pus accumulates. This is called a non-cutting seton.
Diet & IBD
It is clear that not one diet works for everyone with IBD, so it is important to know your triggers, meet with a dietitian and eat what makes you feel good/keeps you healthy.
While you may have a sensitivity or not respond well to some foods, it is not ideal to eliminate entire food groups without consulting a dietitian or healthcare practitioner because you could develop vitamin or nutrient deficiencies. It is important to have a healthy diet because in some cases you already may not be absorbing all of the nutrients from your food, due to inflammation, irreversible damage or a surgery. Even if you have a very healthy diet, you might still need to supplement.
A consultation with a dietitian (who can be recommended by your gastroenterologist) will provide customized information on what you need to improve or include in your diet and how to avoid the things that don’t agree with your digestive system. At first, the dietitian will likely have you keep track of what you eat in food diaries so he/she can see what you might be missing.
Your gastroenterologist or potentially your family physician will likely be checking your blood for deficiencies in vitamin D and iron. While you may be able to improve your levels with diet, some deficiencies might require injection or infusion of large doses to replenish your stores.
If you have a stricture that causes symptoms (abdominal pain, bloating, vomiting), gastroenterologists will usually recommend that you are on a “low residue diet” – this is similar to a low fibre diet – avoiding seeds, the skin of many fruits and vegetables, and uncooked vegetables. Ask your gastroenterologist or dietitian if this is right for you.
To Top